HIV PREVENTION: Researchers dive into finding new ways of increasing prevention innovations uptake | Douches, gels and lubes explored
Madrid, Spain | FLAVIA NASSAKA | A condom is cheap. It’s readily available and has been proven to be over 99% effective if used correctly at not only preventing HIV infection but other sexually transmitted diseases and unwanted pregnancies. But, even with this highly effective tool accessible almost everywhere, the number of new infections are still high.
In fact a 2017 report by UNAIDS put the number of new infections at 1.8million globally. The simple explanation for this is that the “One size fits all” doesn’t work with HIV prevention. Now, researchers attending the HIV Research for Prevention conference 2018 in Madrid, Spain have today, Oct.24 shared findings from studies they are undertaking to explore new avenues through which people can protect themselves from getting infected.
Johns Hopkins University School of Medicine based scientist Craig Hendrix who was delivering a talk about on-demand topical agents for Pre-exposure Prophylaxis (PrEP) which are medications applied either vaginally or rectally by an uninfected person within hours of anticipated HIV exposure said the studies which are in early stages are showing hope of efficacy. So far, according to him eight microbicide products are being studied in clinical trials.
In a study investigators at the US based university did on a douche or enema, gel and manual lube, they found a douche to have 60% retention whereas a gel and lube had 95% and 10% respectively. When it comes to distribution the douche covered 60cms whereas gel was at between 5.9 – 7.4cm and lube rated at 4.4 – 15.3cm.
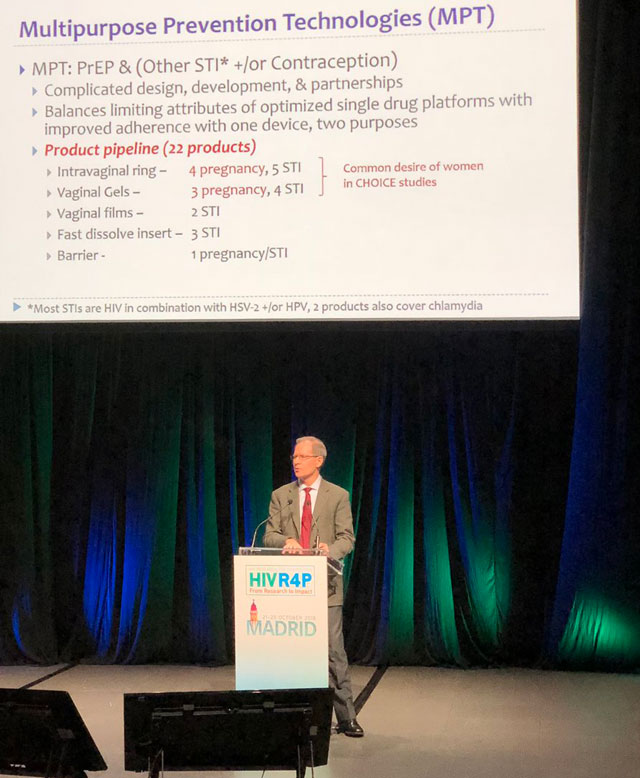
The new products once found effective will add on the list of other new prevention techniques like Oral PrEP where HIV drug Truvada is being used by uninfected people at risk of infection, the injectable ARV drugs cabotegravir for men and rilpivirine for women which are still under clinical trial and early results have showed effectiveness with a jab being given every month and the dapivirine HIV drug laced vaginal ring still undergoing regulatory approvals.
Speaking to journalists this morning, Dr. Nyaradzo Mgodi a scientist from Zimbabwe said the explored options are the best for especially women in the Sub Saharan Africa who may not be empowered at all times to choose protection or not at the time of intercourse.
She however urged scientists to ask people what they really need.
“we don’t know what it will take to end the epidemic that’s why they should ask the end-user what works for them, because if I were pregnant and needed a PrEP option I would choose topical – something that would not go into my blood”. Topical preparations and the ring should be given a try, she said while urging funders who are increasingly investing more resources in systematic PrEP methods like injections at the expense of microbicides like the vaginal ring.
An abstract of a study dubbed ‘POWER’ – Prevention Options for Women Evaluation Research presented at the conference, seem to confirm Mgodi’s view. Done in an open setting in Kenya and South Africa where up to 1000 women were enrolled on oral PrEP Truvada, researchers found that half of the young women stopped using PrEP after one month and one of the reasons cited was disapproval of their medicine use by either partners or parents.
For Mgodi, this is evidence that women can use these prevention innovations if there’s a perceived risk but are sometimes challenged by not having the power to make a choice.
Hendrix agrees. “Ensuring that microbicides are part of the choice is to publically embrace them as pregnant with promise and worth the work”, he said, “Tissue pharmacokinetics is more influential than systematic pharmacokinetics. Time will tell”.
However, as scientists dive into new formulations, Jim Picket of the AIDS Foundation of Chicago asked researchers to start thinking of strategies for implementation even before the studies are complete and approved. For instance he says with all its effectiveness and being approved for use in the US in 2012, only 309,000 people are using oral PrEP globally and 71% are demonstration programs outside America.
In Uganda for instance not much implementation has been done with PrEP being used mainly by serodiscondant couples who access it through research clinics and NGOs.
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price





