It can now be measured. But are we closer to a cure?
The road to a cure for HIV is long, winding, and with no definite end in sight.
That said, a new study published in January in the journal Nature is shedding light on a way to measure what is considered an inactive form of the virus that rests hidden in people’s cells.
This so-called “latent reservoir” of HIV has stood as a roadblock to eradicating the virus, stubbornly staying put despite being attacked by increasingly sophisticated antiretroviral drugs used to treat the virus.
For researchers in the HIV cure field, this new technique is a significant development because it offers a clearer look at how to pinpoint this viral reserve.
Why is this important?
Past tools are said to have greatly overestimated how much of this under-the-radar cache of virus existed in any given cell.
Now, measuring the reservoir to see how it responds to experimental therapies may be less of a shot in the dark.
This new work comes out of the Maryland lab of Howard Hughes Medical Institute investigator Dr. Robert F. Siliciano, PhD, a leader in the HIV cure world. He said that while current drugs out there are doing a good job of attacking and suppressing the virus, none of them are able to get rid of this persistent latent form.
Over the years, Siliciano and his colleagues have attempted various methods to try to get around this problem, essentially “waking up” the latent virus and killing the bad actor cells.
He said, while there are a lot of clinical trials underway to do this, you won’t know whether or not they’re working unless you can clearly measure this drug-resistant reservoir.
“Measuring the latent form is going to tell us whether we are closer to a cure or not,” Siliciano, professor of medicine at the Johns Hopkins University School of Medicine, told Healthline. “You can’t know whether you are making progress unless you can measure before and after an intervention and say ‘Aha, this went down.’ “
Siliciano said that in clinical trials of new antiretroviral treatments, researchers would see just how much the presence of the virus dropped, and whether or not the drugs themselves produced this decrease.
“It really accelerates the development of antiretroviral therapy if you have a simple assay (a lab test used to analyze the effectiveness of a drug, for instance) that measures the key quantity that indicates how much virus is there,” he added. “It should be very helpful.”
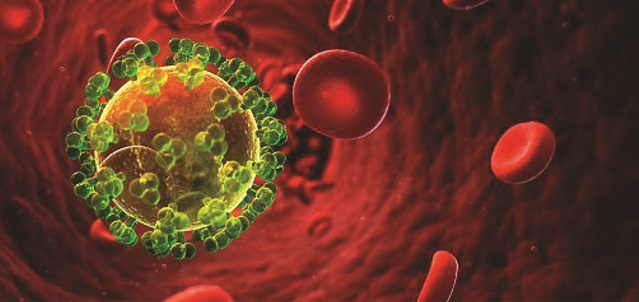
How HIV attacks cells
For those unfamiliar with how HIV attacks a body’s cells, the idea of a hidden stash of the virus evading the attacks of drugs can sound hard to grasp.
Basically, HIV treatments consist of a combination of drugs that hit the virus at a specific stage of its lifecycle. If drugs cut the virus off at two or more of these stages, the virus can’t make copies of itself. It then cannot be detected in a person’s bloodstream.
In 2017, the Centers for Disease Control and Prevention (CDC) announced that people with HIV who strictly stick to their antiretroviral therapies, can reach this “undetectable” viral count.
This means they’re unable to transmit the virus to their sexual partners. While current treatments mean people with HIV can lead healthy, long lives, this isn’t a cure.
The latent reservoir remains stowed away in the genes of CD4 cells, which are what HIV infects.
People who hit “undetectable” status must remain on their antiretroviral drugs because, even when infected CD4 cells go dormant, they hold on to their genetic record of the virus. You might say they’re in hibernation. If a person goes off their treatment, the infected cells wake up and the stored HIV information generates new viruses.
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price





