However, the preventive clothing may increase the cost of treatment
| THE INDEPENDENT | Insecticide treated protective clothing could cut malaria infections in children under five by half while also reducing anaemia rates, a study suggests.
During the study, the clothing, which contained permethrin insecticide, was sewn as a hooded jacket and trouser to cover the child’s entire body leaving the hand and feet at a time they were not under insecticide-treated bed nets in the evening: from five to eight o’clock.
“The prevalence of anaemia at recruitment decreased from 82.4 to 69.6 per cent after intervention,” the study says. “The proportion of those with severe malaria was also higher at recruitment (five per cent) than at second post-intervention screening (2.5 per cent).”
According to a study, children under five are the most susceptible to malaria and malnutrition, with 194 million malaria cases and 407,000 deaths in Africa in 2016.
Researchers say that despite both malaria and malnutrition causing deaths of children under five years old in Sub-Saharan Africa, there is a lack of evidence that preventing malaria could improve nutrition.
The protective clothing was tested among 102 randomly selected children under five, in two coastal communities in Lagos State, Nigeria, for two months, according to the study published in Malaria Journal this month (5 February).
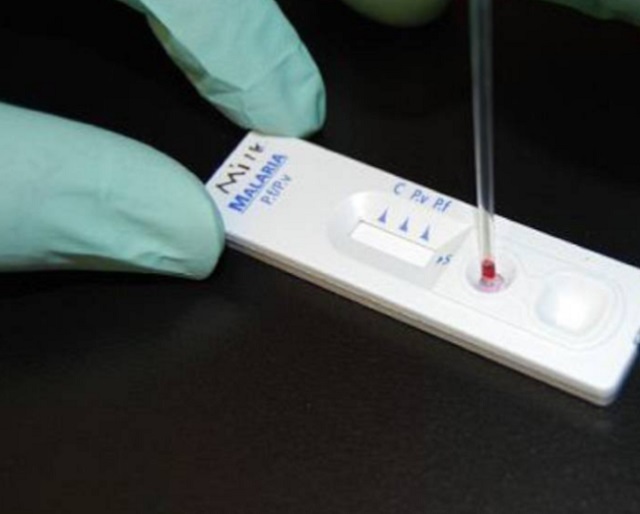
Researchers assessed nutritional status and evidence of malaria before and monthly for two months. They also assessed nutritional status and evidence of malaria before and monthly for two months.
The researchers counselled the children’s parents on immunisation and nutrition while the children were being screened.
Bamgboye Afolabi, the lead author of the study, and chief executive officer of Nigeria-based Health, Environment and Development Foundation, tells SciDev.Net that despite hundreds of millions of US$ spent in Sub-Saharan Africa on malaria interventions, malaria death rates in children under five and pregnant women are unacceptably high.
The study says that Nigeria has more than 51 million cases of malaria resulting in 207,000 deaths annually, the heaviest malaria burden globally. Olugbenga Mokuol, a technical director at National Malaria Elimination Programme, Nigeria, says that the use of malaria preventive clothing is not new.
“For purposes of policy formulation, there will be a need to have a large-scale study. The take home message is that we use nets or indoor spraying as the core interventions for malaria prevention while acknowledging complementary actions such as repellents, preventive clothing, clearing drainage, door and window nets,” Mokuol explains.
“The authors must have chosen that population because of the possibility of using such strategies to give further [clothing] access to the poor,” Mokuol adds.
But Michael Akindele, a paediatric doctor with the Maraba Medical Centre, Karu, a government-owned medical facility on the suburb of Abuja, Nigeria, says that using preventive clothing may have a major challenge.
“The challenge is that it will increase the cost of treatment as each child may be required to have more than one pair of the preventive clothing,” he explains. “How the poor can afford this clothing is something the researchers [should] consider.”
****
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price





