Health experts say their ability to combat infections and save lives are being undermined by superbugs
ANALYSIS | RONALD MUSOKE | The World Health Organization (WHO) has called on world leaders to increase investment in global public health to effectively address critical emerging challenges such as antimicrobial resistance (AMR).
The UNGA79 took place at a critical moment as the world continues to recuperate from the devastating effects of the COVID-19 pandemic.
Speaking at the second high-level meeting on antimicrobial resistance during the 79th United Nations General Assembly (UNGA79) in New York, WHO Director-General Dr. Tedros Adhanom Ghebreyesus, warned that antimicrobial resistance “threatens a century of medical progress” and could return society to a pre-antibiotic era, where treatable infections become fatal.
“This is a threat for all countries, at all income levels, which is why a strong, accelerated, and well-coordinated global response is needed urgently,” Dr. Tedros emphasized, stressing that global action is critical to avoid a regression in modern medicine.
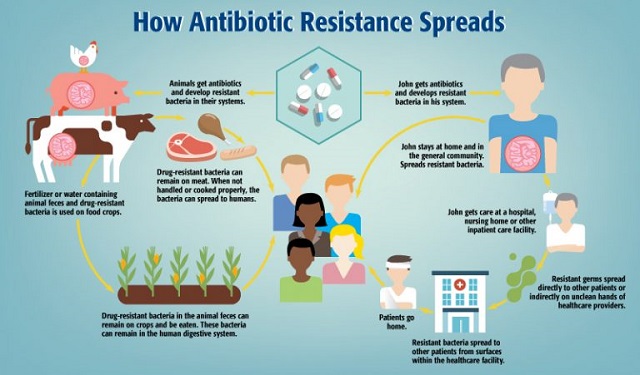
According to the World Health Organization, antimicrobial resistance happens when pathogens such as bacteria, viruses, fungi and parasites change over time and no longer respond to medicines making infections harder to treat, hence increasing the risk of disease spread, severe illness and death. The pathogens that develop antimicrobial resistance are referred to as “superbugs.”
Donors sound alarm on superbugs
Donors who support public health sytems around the world also sounded the alarm on the urgent need to address anti-malarial drug resistance during the UN General Assembly. In their joint statement, the donors noted that although widespread use of artemisinin-based combination therapies (ACTs), which combine artemisinin with a partner drug, have contributed to tremendous reductions in malaria cases and deaths over the past two decades, the recent emergence and spread of ACT drug resistance in Africa is now threatening progress and putting millions of lives at risk, forcing malaria endemic countries to stop or scale back other life-saving malaria interventions in order to buy more costly ACTs.
The donors said evidence of resistance to the artemisinin component of ACTs has emerged in several locations including Rwanda, Eritrea, Ethiopia, Tanzania and Uganda.
AMR is significant development challenge
Dr. Jane Ruth Aceng, Uganda’s Minister of Health, told a high-level meeting on antimicrobial resistance in New York on Sept. 26 that antimicrobial resistance is a significant development challenge, which is undermining progress made in combating diseases like HIV, tuberculosis, hepatitis, Ebola virus and malaria. She was speaking on behalf of the G-77+ China Group.
She said the rise of drug-resistant bacteria threatens these efforts and could lead to increased mortality, healthcare costs, and worsening inequalities.
Dr. Aceng said the G-77 strongly urges the international community to recognize the damaging effects of unilateral coercive measures on the ability of developing countries to combat anti-microbial resistance. Such measures, she said, limit access to antimicrobial medicines and weaken health systems.
“Many developing countries in our Group have demonstrated strong commitment to tackling antimicrobial resistance by aligning national action plans with the World Health Organization (WHO) Global Action Plan and endorsing the UN Political Declaration on anti-microbial resistance,” she said.
Dr. Aceng noted that in Uganda, the government’s response to antimicrobial resistance is being guided by a comprehensive national action plan, which is grounded in the “One Health framework (looking at humans, animals and the environment).
“It emphasizes strengthening diagnostic capacities, infection prevention and control strategies, enhanced anti-microbial resistance surveillance, prudent antibiotic use, and strong collaboration,” she said during a meeting co-hosted by the South Centre and the Permanent Mission of Uganda to the United Nations.
Dr Aceng noted that significant challenges remain, particularly in accessing affordable antimicrobials, vaccines, diagnostics, and other health technologies. She said financial resources to implement these plans are insufficient. “We welcome the target of mobilizing US$100 million through the Antimicrobial Resistance Multi-Partner Trust Fund to ensure that 60% of countries have funded action plans by 2030,” she said.
Africa’s alarming cases of AMR
According to a recent report published by the Africa Centres for Disease Control (Africa CDC), the likelihood of falling ill or dying from diseases that resist treatment has escalated in Africa, with children and other vulnerable groups being most at risk.
“The continent faces the highest mortality rate from antimicrobial resistance, with 27.3 deaths per 100,000—exceeding the combined death toll from HIV-AIDS, tuberculosis and malaria,” said the “African Union Landmark Report” launched on Aug.15 at the Africa CDC headquarters in the Ethiopian capital, Addis Ababa.
Africa bears a significant burden of infectious diseases, accounting for about 95% of malaria deaths, 70% of people living with HIV, and 25% of TB deaths globally, said the report.
“We must not ignore this silent threat that disproportionately impacts the most vulnerable among us,” said Dr Raji Tajudeen, the Africa CDC Deputy Director General.
Health experts say the continent requires between US$2-6bn every year to effectively respond to antimicrobial resistance. However, current funding is only a tenth of that allocated to other major diseases.
The underfunding makes antimicrobial resistance a significant barrier to sustainable development, hindering progress toward the Sustainable Development Goals (SDGs) and the African Union’s Agenda 2063.
An estimated 700,000 people die annually from drug-resistant infections globally. Without timely intervention, this number is projected to reach 10 million by 2050, with Africa accounting for 4.5 million. “Fighting disease requires resources and working with member states and our partners we need to do all we can to save lives,” said Dr Tajudeen, speaking at the launch of the report.
Dr Huyam Salih, the Director of the African Union-Inter African Bureau for Animal Resources (AU-IBAR), emphasized the critical role that the AU must play in combating anti-microbial resistance.
“Antimicrobial resistance is not just a health issue—it is a threat to our agrifood systems, food safety, food security, livelihoods, and economies,” she said.
By 2050, global healthcare costs could exceed US$1 trillion per year, and livestock production could decline by 2.6% to 7.5% annually due to anti-microbial resistance, according to Dr Salih.
“In Africa, the situation is particularly alarming, with 37 countries reporting the prevalence of anti-microbial resistance in animal farms, yet only 16% of African countries are conducting routine AMR surveillance in animals as of 2023,” she said.
She also called for urgent action to strengthen leadership, expand surveillance and data systems, promote the responsible use of antimicrobials, improve public and animal health systems, and secure sustainable financing to combat anti-microbial resistance effectively. “Our health, our food, and our future depend on the actions we take now,” she said.
Dr Tajudeen said addressing anti-microbial resistance in Africa requires engaging all levels of society in a comprehensive and multi-sectoral approach. “Unless we work together, overcoming antimicrobial resistance will be a difficult and long-drawn process that will cost lives,” he said.
Currently, millions in Africa lack access to essential antibiotics, with a study by Africa CDC and the African Society for Laboratory Medicine revealing that only 1.3% of microbiology labs in 14 member states can test for key anti-microbial resistance pathogens.
Nqobile Ndlovu, the head of the African Society for Laboratory Medicine noted said his organization is “committed to strengthening African laboratory capacities to combat antimicrobial resistance. “Our goal is to ensure the continued efficacy of treatments and promote data-driven solutions to safeguard public health across the continent,” he said.
Climate change escalating challenge
Appearing on a different panel at an earlier side event on the same topic during the UN General Assembly, Dr. Diana Atwine, the Permanent Secretary in the Ministry of Health emphasized the importance of regulation and investing in risk communication. She said people at the community level seem not to appreciate the problem of anti-microbial resistance.
“People are (easily) accessing medicines and there is irrational use of anti-biotics. They can access the anti-biotics anyhow; they don’t complete the dose; there is no strict regulation or information out there. If we are going to strengthen and reverse anti-microbial resistance, we need to get strong regulation in the country,” Dr Atwine said.
“We need to understand that anti-microbial resistance is a big-time bomb for us and we must all commit. And commitment is not about how many meetings we hold; it’s not about how many presentations we make; it’s about what we are going to do as individual countries differently.
“Anti-microbial resistance is a global health issue and when we talk about global health security anti-microbial resistance comes to the fore. If, right now people got serious streptococcal, a serious resistance strain, it can be an epidemic and it can wipe out a generation.”
Dr Atwine also sounded the alarm about climate change that, apparently, appears to be escalating the problem of anti-microbial resistance. “Whether you want it or not, climate has contributed to anti-microbial resistance,” she said.
“Even if you have very good systems and good protocols that you adhere to prescription practices, the bacteria are also invading nature; they must survive,” Dr Atwine said.
“In Uganda, the viruses that we are isolating right now are unprecedented, so climate change is also a big driver. We must also deal with the pressures that is being put on viruses, the fungi and protozoa.”
Dr Atwine also noted that if anti-microbial resistance is going to be tackled decisively, research and development should not be left to pharmaceutical industries alone. She said the academia must step up to the forefront; go on the ground, do the research and come out with the data.
“This data is then presented to the national policymakers saying this is the problem; this is where we are and this is a time bomb.” “After looking at the data, then we come up with a response plan starting with the communities.
For Dr Susan Nabadda, the Commissioner for Laboratory Services in Uganda’s Ministry of Health, the need for countries to prioritize and fund diagnostics so that they can have strong diagnostic capacities with short turn-around time of results to support clinical decisions and prescriptions could also go a long way in the fight back against antimocrobial resistance for countries like Uganda.
A call for a comprehensive action
In New York, Dr Aceng said antimicrobial resistance control strategies must include improving water, sanitation, and hygiene (WASH) systems in healthcare settings and communities. She said infection prevention, supported by reliable WASH infrastructure, is crucial to reducing the spread of drug-resistant infections.
“Strengthening regulatory frameworks and promoting appropriate antimicrobial use across all sectors must be prioritized through increased investment in innovative, rapid, and affordable diagnostics,” she added.
The G-77+China coalition believes that overcoming antimicrobial resistance will require concerted action in areas such as mobilizing sustainable financing and investment for developing countries through innovative mechanisms for long-term antimicrobial resistance initiatives; strengthening governance structures for antimicrobial resistance control using a whole-of-society approach.
The coalition also thinks improving supply chain management and removing trade barriers while fostering collaborative manufacturing of antimicrobials, diagnostics, and vaccines for equitable access as well as strengthening surveillance systems for anti-microbial resistance and antimicrobial use to support the collection of national data and promoting research and innovation to develop local and regional manufacturing of new diagnostics, antimicrobials, and vaccines could help improve the situation.
 The Independent Uganda: You get the Truth we Pay the Price
The Independent Uganda: You get the Truth we Pay the Price





